A lot has been on Dr. Taite Anderson’s mind since he reopened his practice. Like clinicians across the country and the world, this respected oral surgeon from Granger, Indiana, is adjusting to a new routine and is having to think differently about how he approaches patient care. Here, he shares his thoughts on how the coronavirus pandemic has changed him, his team and his practice.
Day 1: Coming Together as a Team
As I reflect on my first day back, I felt such a mix of emotions. I started off yesterday’s morning huddle with a different question than usual. As I looked at the “special ops” team around me, something was different. I thought they were feeling it too. So, I asked them.
“Anyone else feeling it? I feel like I have this pit in my stomach. I am a bit nervous. It seems silly to me, but I still feel it.”
Engaging with eye contact, they each individually nodded. We all felt it.
“Kinda funny, right? We have been doing this so well for so long. But here we all are, nervous about today,” I said, feeling better that it was finally out there. “This is the place we are supposed to be. We are here on purpose. And it is OK and even good to be a bit nervous. There is a lot we don’t know about this whole COVID thing. Some of what we thought we knew has changed. We have our systems in place, and we all know what to do. So, let’s saddle up and do what we do best.”
I really was nervous. My mind was racing with the kind of questions that don’t feel good:
Are we being safe enough?
Is it right to be opening up for elective cases?
Will this put people at risk?
Can I afford to be fully staffed already? I don’t have the plasma ionizers installed yet. Should I wait until they are functional before seeing more patients?
And then there are all the questions that feel a lot heavier about my family and how everything is going on that front.
But we had a plan. We are on the 14th version of the plan according to Rebecca, my office manager (team leader). Her role around here is to give wings to the vision and roots to the values. And she does just that with discernment and resolve.
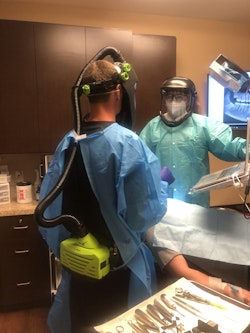
We had all the PPE lined up, reworked the patient flow, studied the recommendations and were doing our best to be safe. Also, to look and feel safe.
It All Starts with My Team
I am convinced that, of all the people, it’s most important for my team members to feel safe. They need to know and believe that I want what is best for them and their families. I have done my best to educate and engage them on redesigning the flow and re-engineering the system in this new Wild West.
I have a few friends who are dealing with staffing issues in their practices. Their hygienists are unwilling to come back to work because they are afraid. When we were talking as a group, they wondered how they could convince their hygienists to come back to work. My response was this: “If your team doesn’t feel comfortable in your office, they will be your worst enemy when talking to their friends and your patients. What would it take to get them comfortable with coming back to work? If they feel safe, your patients will return. If they don’t, you won’t have to worry about convincing your team to come back because you won’t have any patients. How can you work with your team to use their knowledge and perspective to be and feel safe?”
That has been a guiding question for me during this time. I want my team to know I will protect them and lead them even when the rules of the game keep changing.
Learning to Interact in New Ways
I apologized to a patient today when I was just starting surgery. “Sometimes I think my scuba suit is like my shower… I can sing as loud as I want, and no one can hear me.”
Graciously, when surgery was over, she complimented me on my singing. There has been more positive feedback on my singing and humming during surgery than I could possibly have imagined 10 years ago. I have had countless patients comment on how it made them feel more relaxed. And some say they started to get nervous when I stopped singing during the surgery. Of course, I say I didn’t know the rest of the words to that song…
There are two things I hate about how COVID-19 is impacting my office. I hate not being able to shake the hands of my patients and their people. That bond has been taken away. And I hate how much more challenging communication is with all this PPE on. When fears about the pandemic were beginning here, I bought a bunch of durable PPE. I didn’t know what was coming down the pike, so I bought a variety of viscoelastic half face mask respirators with p100 filters, clear welding face shields, a few PAPRs… I wanted to be able to reuse all the critical PPE arsenal for my office. And I was legitimately concerned that my wife and I would be called to duty as make-shift intensivists at our hospital. That was a stress among other stresses of the pandemic.
As we began to work through the challenges of caring for patients with emergencies, I felt like a clown in my new suit. I had a big face shield, scrub cap, gas mask and gown. Everything in the room was covered in plastic.

The first surgery I did during the lockdown was to remove five implants, biopsy and debride the anterior mandible and perform incision and drainage on what proved to be a severe case of osteomyelitis. And I did it alone, without an assistant. This was five weeks ago. I was scared and didn’t want my team or anyone else unnecessarily exposed to this new threat. My friend Patrick was at the office, ready to help. His partner had placed the implants six weeks before and he graciously offered to join me in case I needed any help with the prosthesis.
Since that first surgery, we have gotten quite a bit more comfortable with the new routine. But it was scary not knowing what we were dealing with. I now wear my scuba suit for all my surgeries. Not because I feel I need the powered air purifying respirator with the incredible HEPA filtration. I wear it because my patients can see my face and hear my voice. The other masks and shields make it so difficult to hear and completely take away real communication.
So, I put on the belt, hose and full-face mask for every surgery. God, I hope I can find a better solution soon. But I find the connection with my patients and my ability to meet them where they are at and calm their fears is worth it. Even if the singing is a little off key…
At our routine weekly team meeting, the agenda had only three items in new business:
1. Yesterday
2. PPE
3. Check-in (patient flow)
We set a record today for the least items on the agenda. By far.
We’ve had multiple Zoom meetings, but we were finally able to sit around the conference table together, with masks on of course. It was wonderful. I got the same typical head nods and team interaction that have become the norm for Tuesday mornings. We spent time going around the table, each sharing what we are thankful for. This is one of my favorite things to do as a team, so we do it quite often.
“Joy is the fruit of gratitude,” I say as we finish sharing our thanks. Then it got real. I shared the following:
“This has really sucked. It has been hard and stressful. We all have our own stresses. It may seem like one person’s stress is more than another’s. But we have all been challenged in new ways and our brains have each handled it as they were designed to do: with a stress response.”
So, we spent some time as a team sitting in the weight of what we have come through and where our journey has yet to go. We paid honor to the challenges and the tough feelings. I don’t mind the awkward silence. We talked a bit and then sat in it. It was good. We all wished we could have done things a bit differently over the past six weeks. I sure would have loved to have been more intentional about some things. But as a team, we sat in the tough past and the tough future, and decided we wanted to keep moving forward, even if the steps we were taking may not be perfect.
The team, in their typical head nod way, agreed that we can look back on the past six weeks and know we have made it through some tough times. We stuck together and we are better for it. I am thankful I was able to put my money where my mouth is when it comes to their value to me. We marked the time in history as a team, and we took a step forward. We did what we had decided to do, and the day began.
Searching for Solutions
I have this problem. It may be only one of many, but it is the one I am facing most clearly right now. You see, I sometimes I have an idea that I think just needs to come to fruition, so I throw myself into it full throttle. Sometime in the past six weeks, I got to thinking about why dentistry is such a risky business in the COVID-19 era. When I thought about the aerosol generation issue, I figured there must be some good solution. I don’t know exactly how this obsession began, but I have been convinced, for the past few weeks, that if we just run diluted hydrogen peroxide through the irrigation lines for ultrasonic scalers, highspeed handpieces and air water syringes, the SARS CoV-2 virus will generally leave dentistry alone worldwide.
Initially, I thought this deserved a patent. I thought I had this gazillion dollar, “novel” idea that just needed a bit of work to flesh out.
At this point, I have resolved that my problem (aka my idea) has no significant monetary value as hydrogen peroxide cannot be patented and marketed. So, I have taken the more noble route and am desperately trying to figure out how corrosive a 1% solution of H2O2 is to a dental unit. I have also been elbow-deep in articles and research regarding the impact of airflow and ventilation on dentistry in the COVID-19 era. It is difficult for me to focus on some of the daily tasks when the salvation of dentistry from the coronavirus pandemic is on the line.
My team is amazing. They believe in me (or at least let me believe they believe in me). They think. They care. They perform. They are Granger Oral Surgery. We’re not perfect, and that is why it works.
Moving Forward
The questions plague me. But I have learned they can be my guide as we continue to move forward.
Is it safe?
Is it possible?
Is it reasonable?
What is the real problem? And what are other peoples’ solutions? What other solutions might be out there in another field that we could tap into? What other solutions might be waiting to be developed?
Is it the best?
Does it communicate value and worth to my team? Patients? Family? Myself?
Given my history, my future hopes and dreams and the current situation, what is the wise thing to do?
Despite all the questions, we have made it through the first few days. Day 2 was over 52 minutes ago. We successfully received disbursement from a PPP loan, rehired the team to full time, implemented a whole bunch of new PPE SOPs, regrouped as a team, took wonderful care of patients and marked day 2 of the return. It wasn’t perfect. It was clumsy and awkward at times. We dealt with new questions and problems. But we did it together, as a team. And I am so proud of the team I am on. I am so thankful to have their trust and that they put it all out there.
Day 2: Today Feels Different
My wife, as a primary care physician, has been watching the crisis unfold since she first learned of this new threat in December. One guiding principle for us has been this: It is impossible to regret being too cautious. If we get through this and it wasn’t as bad as we thought it was going to be, then we did just enough. Regret can only rear its ugly face if we look back and wish we had done more.
So, when I have a patient clearly feeding me a line because he wants what he wants (and we all know when the motives are just so), I used to be able to play it off and have my team get the patient scheduled. But now, I am in the middle of trying to figure out if my desire to serve people in their time of need could potentially cost me dearly. I feel like the rules have changed. The game has changed.
I used to be delighted when something new and challenging popped up. Now, I question how to handle pulpitis versus apical periodontitis versus an acute abscess. Which is an emergency? Which patients really need me right now? And if it is an emergency, do they really need to be sedated for the procedure? These questions used to be so easy to answer. When I got paged, I went in. No matter what. Now, well, I am left wondering if the antibiotic Band-Aid will be enough.
But today feels different. The governor of Indiana has released us to begin providing elective services, as long as we are not depriving the frontlines of their needed PPE. So, my team and I have done our best to understand what this sub-micron enemy is capable of. We have upheaved the system we spent years honing and refining. We have considered and reconsidered how to don and doff. Where to don and doff. What exactly are we to don and doff? And does that mean between every patient? Even if I just go in to say hello?
As we officially opened for business today, it finally feels like we can re-enter some form of normal. But I am scared because I don’t know if the horrors of what I hear and read and see are somehow going to happen here. My wife and I got married right before medical and dental school. We have been together through thick and thin. She is my rock. But now, when we finally feel like we know what to do or think this “something” might make a difference in this new battle, the rules change again. So, while I would like to be able to look back at this time and think we were entering a new normal, right now, I just want to know what I am doing is good enough.
It happened. I saw patients, face (mask) to face (mask) today. No webcams. We were all a little sheepish. Some patients obviously thought everything in the world was an overreaction. Others were legitimately concerned for their own health and safety. Humanity entered my office today, just as it has for years.
But it was more exposed. People are often quite nervous to visit me and my team as we are Granger Oral Surgery and Dental Implants. We get to meet people in their time of need and vulnerability. But now we are just as vulnerable. And the ones who act the least vulnerable are our greatest risk. My how the rules of this game have changed.
My mind has been running non-stop. I need peace and rest. I worry about my family, my friends, my country, my team, my practice. I have said countless times to so many people who know me well: “I am still me. I am the eternal optimist. But I am seriously concerned.” When the eternal optimist is worried, that says something. Am I just overly concerned? A hypochondriac? No. This one is real.
Sometimes what is urgent or emergent is in the eye of the beholder. Sometimes it is in the hospital pager. Other times, all we can do is what seems like the right thing and hope that if we missed it, it wasn’t a true emergency. As I sit in my home tonight, reflecting on this wild and crazy time, I’m just thankful to be here and to be well. When asked if my glass is half full or half empty, I would always emphatically reply with “overflowing.” Right now, at this moment, I am just thankful to have a glass.
Day 3: Dealing with the Grief
We all cope with frustration, disappointment, and grief in different ways and on different timelines. I have found that my patience is most thin when I think everyone should be thinking the same way I am.
Everyone is experiencing some measure of upset right now. For many in the world, it is the loss of a loved one. For others, the loss of a job. For my kids, it is disappointment that looms larger because of their ages. It’s the cancellation of the annual spelling bee or the spring soccer season or denying the promised birthday celebration.
My amazing daughter recently turned 9. For her golden birthday, she was going to spend a day with dolphins at an aquarium in the Keys. We were all so very excited about our planned journey. This certainly is smaller than most losses in this time of grief, but it is significant to her and to us. And when you're 9 and your world seems upside down, it is understandable that frustration and disappointment cause you to dissolve into tears.
Part of why we are all at different places during this time may be because we are in different stages of grief. I keep thinking that my team must be handling things a bit differently than I am handling them. I was thrust into this thing headfirst and have had to deal with the reality of the changes right away. I try to be sensitive to my team and patients as they may be in a different state of mind. It may take them longer to feel comfortable because they haven’t processed things like I have been forced to process them.
And for that, I do not dislike them. Rather, I try to dig deep and find opportunities to meet them where they are and not expect them to be anywhere else. That gives me peace. The mind cannot unlearn. It seems to me like it takes practice to be able to empathize with a fellow sojourner who has not yet had the opportunity to take as many steps in the journey. I have often heard that practice makes perfect. I believe that practice makes progress. That feels a lot better to me.
Day 4: Gaining Perspective
I have been learning about comparative suffering: keeping our struggles in perspective while allowing ourselves to feel and express them. As mentioned yesterday, when my daughter’s brain is going through the trauma of the loss of what she knows as normal and the loss of things she has been hoping for, her autonomic nervous system and lower brain are going through the universal process of grief. I realize that though her grief may be different in perspective, this has been one of the hardest times in her life.
Our struggles may seem bigger. Her struggles are real too. Sometimes, I find it difficult to respect other people’s struggles when my own seem bigger. Yet it is that confluence of perspective and respect that fuels empathy. So, I try to see my people. I try to understand their fears. I try to meet them where they are. I try to allow myself to feel, which sometimes seems like the opposite of what I was trained to do. This has helped me find tremendous empathy for myself and others.
On Monday, I was running 7 minutes late for my evaluations. Clara came to me with a problem and I was supposed to have the answer. Her left mandibular torus was exposed and sore and she needed it removed. Simple. I can do that.
Yesterday, her husband was sent home on hospice. Her pain was multiplied by the five days he was hospitalized, and she was unable to visit him. He was alone. She was alone. I listened. I saw. I felt. My eyes welled up. My heart was with her. I met her and gave her permission to take care of her husband and herself and to address the simple problem that brought her to me when she was able.
It felt cold to not offer a gentle touch of comfort or even to shake her hand before I left. She couldn't afford to get sick. I don't like thinking about it that way. I guess this is part of the new normal. And before I knew it, I was out the door and on to the next patient. Sometimes I find I can only be my true self when I take the time to see others as their true selves.

Day 5: The Space Suit
No one knew how things would play out returning to work. I knew there were limited supplies worldwide and that a powered air purifying respirator was the ultimate in personal protective equipment. While I hoped for the best, I wanted to be prepared for the worst.
There was no way I would protect myself better than my team, so I ordered two Optrel e3000 Clearmaxx PAPR units in the beginning of April. They have become known around my office as my “scuba suit.” At the time, it felt like they would be a last resort bailout for the worst-case scenario. After trying a dozen combinations and modifications of masks and face shields over the past month, the scuba suit was born. I drilled holes in the face shield of the PAPR to mount my Snap On Optics light in line with my loupes. I belted on the blower and headed in for surgery.
Challenging upper left third molars and direct sinus lifts always seem to aggravate my neck and back the most. After back-to-back sinus lifts and two difficult sets of adult impacted thirds, my neck was on fire. The weight of the headgear and the belt was too much. There had to be a better way. So, I started to hang the blower belt on an IV pole and drag it around with me. It is more awkward to navigate with an umbilical cord attached to an IV pole but removing that added weight from my back has been totally worth it to me.
One of the goals in my practice is for patients to not feel any pain at my hand. The hygienist and nurse on my team are totally amazing at administering local anesthetic and starting IVs. They are skilled, compassionate and patient. When I walk in the room all suited up, the patient is ready to start surgery.
“I brought my scuba suit today,” I announce with a warm smile on my face. It has been very well received overall. But it sure is awkward at times dragging along the short IV pole. I get flashbacks to my recovery after my appendix ruptured, toting my IV pole around the halls. We definitely joke about it as a team. I have embraced Brené Brown’s quote: “Stay awkward, brave and kind.”
I continue to think of ways to improve things. Recently, I ordered a 3M Versaflo M-107 assembly and modified it to work with the Optrel blower. My team coined it the “space suit.” I find it more comfortable. It fits my head better. The hose attaches at the back of the head and that seems to balance the weight better. Airflow can be adjusted some, but the only supply is at the top of the face shield. That dries my eyes out a bit more than the Optrel, which has adjustable vents at the top and bottom of the face shield.
Currently, I am using my space suit for every surgery. I make small steps every day, constantly getting better at what I am doing.
The products:
Optrel e3000 Clearmaxx Approximately $1,200
Day 6: Adapting to Change
My dad finished dental school right before wearing gloves in dentistry was mainstream.
“I remember one time eating a piece of toast after work and smelling my last patient’s mouth, even though I washed my hands multiple times,” he told me a few weeks ago. Thankfully, we have adapted to that change. I hope to look back at this time in 30 years and see some humor in how things have changed. What will our kids be appalled to find out we didn’t do before this time? What will we laugh at when we realize how vital we thought something was that proves to be completely pointless?
The processes improve. I spent 7 years building and refining a system and flow in my practice and I found myself worrying it was all going to have to be redesigned. Yet we are getting more used to it. And we are improving the processes. As the routine is settling in the flow is becoming more fluid. It had muddied up some possibly because of the hiatus and disuse, but mostly because of the changes. And I truly hope for more changes yet.
I keep thinking it has to get “better.” Sometimes “better” feels like clarity on safety requirements. Sometimes “better” just seems like easier and more comfortable PPE. Whatever better will be, I welcome it and am looking for it.
After a terrible back and neck ache last Friday, I started hanging the belt of my scuba suit on an IV pole that I cart with me into each room. I also have been more acutely aware of how critical good posture is with the added weight of the equipment. Yesterday, after bilateral direct sinus augmentations, multiple extractions and ridge augmentation on my brother-in-law at the end of a busy day in the clinic, I was tired mentally and physically. But my neck and back felt much better than last Friday when I spent the day wearing the belt.
The little changes keep making it more comfortable and easier. If I sat for surgery, it seems like it would be even more comfortable. Without trying something, I don’t know what to change. I can’t very well improve what I am doing until I start doing it and pay attention to what seems good and what needs to change. When I give myself permission to shift from thinking and overthinking to doing, I often find the answers show up right in front of my face. And I wouldn’t even have known there were problems if I hadn’t got busy doing.
Maybe this is what everyone is talking about with the “new normal.” After only a few days in the clinic, there is a new rhythm forming. The new normal is what people seem to call it. But it feels a lot like the old normal with just a bit of a twist.
Our course may have been altered recently by this storm, but it has not changed true north. We have all changed. We are more seasoned. We are a tighter unit. But it feels more like the old than I was expecting.
Some of the “new” things may just be things that should have been all along. My hands are getting sore as I have more than doubled the number of times I wash them or use hand sanitizer. Cleaning the door handles throughout the day may have been a good idea all along.
The reality is, not that much has changed in my practice. Not nearly as much as I had envisioned. With how things were progressing in mid-March, it seemed like everyone was going to need hazmat suits just to go outside. Now, with a few noticeable and some unnoticeable changes, we are doing as much surgery as we did before the pandemic struck. It feels like we are still revising all the recent changes daily: clinic flow, check-in from the parking lot via text, doling out masks to patients who didn’t wear their own, constant facility cleaning, changing how we hold the suction to reduce aerosol…
I wonder how important the changes that go unnoticed will prove to be: increased ventilation, plasma ionizers, HEPA filtration. It seems like they are getting a lot of attention and we are all throwing a lot of money at them.
Day 7: Through the Wave
The storms on the Great Lakes have been earning my respect since I was a child. They can blow up seemingly out of nowhere. I vividly recall getting caught in four. Two on Lake Superior as a young sailor under my father’s steady hand and two on my own vessel responsible for my own precious cargo.
The lessons I learned sailing with my dad in the Apostle Islands on Lake Superior helped shape me. Sure, I learned about battening the hatches, reefing the sails and securing the galley for the squall that was announced on the monotone weather radio. But when the black band forming between the indistinguishable grays of the water grew and swallowed the sky, my brothers and I were enthralled by the big waves and waterspouts around us. I don’t know what my dad was feeling, but his calm smile and distinct laugh taught me how I wanted to navigate the storm, with calm, fascination and joy.
I didn’t know it at the time, but what he taught me and my two brothers on our annual sailing trips went far beyond “The Annapolis Book of Seamanship.” It made us who we are.

Painted by Dr. Taite Anderson while quarantined.
When the spray of the waves slaps your face all the way back at the helm and the wind threatens to tear the standing rigging to shreds, through the waves and into the wind is the only hope of safety. You must keep your eyes on the horizon as the waves threaten to disorient even the most experienced skipper. You must look through the waves to the horizon and you must keep forward momentum so your vessel doesn’t get turned sideways and risk taking on water or capsizing.

Dr. Taite Anderson’s Father
My internal dial seems to be shifting from some level of fear to respect for this new formidable foe known as coronavirus. I was never taught to fear the storms, though that may come naturally. I was taught to respect them. I don’t set sail in the storm, but when they come, I do my best to bless those on my vessel with the same calm and joy I see in my father.
A smooth sea never made a skilled sailor.
Day 8: Cooking Bacon
The process of personal protection is universal and innate to humanity and to all living creatures. It has been described as survival of the fittest, adaptation, evolution. This has been constant since the very beginning of life itself. The living creature needs to survive.
Today, I realized I was using the same principles of protection when I cooked some delicious bacon: ventilation, shield, gown, gloves.
I cranked up the hood ventilation over the stove before the bacon hit the skillet. While I love bacon and enjoy the aroma, I didn’t want to drive my family out from the smoke. As it began sizzling, I held the lid to the pan in my left hand as a shield from the molten splatter and flipped the bacon with the protection of an oven mitt and tongs in my right. My apron got a little more seasoned today as the grease splattered on the words “I’d smoke that” and picture of a pig. I just chuckled and reminded my family how big of a nerd I am when I shared the commonalities of cooking bacon with our approach to PPE at the office. The difference being I was solely responsible for cleaning up the greasy stove after it was over.
To be successful, you must be able to fail without feeling like a failure. I struggle with that. I especially struggle when the failure disappoints someone. During the shutdown, I felt like there were enough other disappointments that if I disappointed someone, it was just another drop in the bucket. I didn’t feel personally responsible if we couldn’t meet a patient’s timeline. I also didn’t have any implant failures during that time. I didn’t realize the peace I had until this week.
I felt the sting today when I had to remove an implant I placed on a lovely young woman who feels like her life has been completely flipped upside down. Her tears of disappointment were amplified by the stress of this pandemic: missing the last part of her senior year. No graduation. No senior backpacking trip. No senior party. This is the most stress she has ever been through. I didn’t realize the peace I had during the shutdown, but I didn’t have any surgical failures present during that time.
As much as I think I should be able to see these things as opportunities for improvement, it is still a heavy stress for me. The pandemic seemed to level the playing field. We were all in the same boat. Somehow, I felt like the bigger enemy out there made some of the smaller issues disappear. The old stresses seem to be happy to return as the rhythm of life resumes. I wish I could take the good parts of the quarantine and mix them with the good parts from before the pandemic.
When I agreed to do a brief interview with our local news station, I thought it would be easy to talk about what we are doing to be safe. The reporter was particularly interested in our PPE usage. Our arsenal runs the gamut from the typical masks and gloves to the P100 and PAPRs.
When we were setting up for the interview, I realized the complexity of what was unfolding: in a polarized atmosphere and with little true science to guide us, I was trying to communicate to the general public the safety of dentistry, which has been declared one of the highest risk professions in this pandemic.
My hope was to provide a sense of calm and safety around coming to my office. I didn’t want to scare people away or intimidate them. Some will be comforted by the additional personal protective equipment and others terrified by it. Some may expect their dentist to have the same equipment and protocols. I want unity. I don’t want people to fear any more than they already do. I certainly don’t want to add to their fear.
There seems to be a significant divide in the country regarding the pandemic and the response to this new threat. My goal was to calm and unify with my words. I think it was successful. I hope it was.
Day 9: Smoke Follows Beauty
You could feel the warmth of the fire on your bare, sand covered toes. The sporadic cracks of the burning wood broke the trance the flames had placed over you. It was summer. The campfire aroma embedded itself into every thread of your clothes and every pore of your skin. Grandpa Tom was like the gentle master of the summer evenings, as the dusk faded into the starry night over Lake Michigan. The single threat to the peace of the summer night was the sting of the smoke as it bathed your nostrils and eyes. All it took was the slightest change in the breeze and there it was.
“Smoke follows beauty.” He would say as his face and eyes emanated wisdom and adoration. It didn’t make the smoke go away. The sting of the smoke resolved with the musical chairs so common around a campfire. Something valuable was eternally etched into my wife’s core from the time she was a young child around the campfire with Grandpa Tom. It is hard to know the power and impact of the constant love and wisdom of a grandparent. He was a good man. One of the best. His legacy of love and wisdom lives on in his amazing children, grandchildren, great grandchildren. Now when we are sitting around the campfire with any descendants of Tom Krug and the wind shifts even slightly, Grandpa Tom’s words are sure to be quoted. His spirit lives on.
It doesn’t take much of a breeze to carry submicron particles. If you have ever played campfire musical chairs, you know what I mean. If you are upwind of the fire, you almost don’t even smell it. Even if it is just a slight breeze. What matters is the directional flow. When my mental picture of aerosol changed from spray paint to dental work, I started to think about things in a different way. Yard work was one of the things first on my pandemic lock-down to-do list. As I lit what remained of last year’s sticks and leaves, I could so easily picture and much more practically understand why directional flow was so important in the new era of dental safety; the aerosol carries our nemesis and the direction of the airflow carries the aerosol. I started to think more about where my air supply and return were in my operatories. My mind was distracted looking for information. I turned my attention to google, populating my search bar with “aerosol,” wanting to know more about how it impacts our safety.
I will admit the nerd in me was a bit giddy when my particle meter arrived. I had to know more about this. My curiosity cost me $120 this time. My team has embraced my little homegrown experiment. Just like a toy at Christmas, I couldn’t wait to try it. I opened it, turned it on and pressed “run” before reading the instructions. The numbers didn’t have any real meaning to me, but I started writing them down. As I did my notes at my desk, I ran it several times. Apparently, the air at my desk has around 3000 particles 0.3 microns per liter and rarely any measurable particles 2.5 or 10 microns. I was admittedly startled when it jumped to over 40,000, 20 and 0. It took me a second to put the pieces together, my mind asked what felt like a hundred questions. My gaze automatically goes to the woods behind my office when I am thinking at my desk. I am sure I had on my thinking face (which I have come to realize looks a lot less pleasant than I wish it did. The way my brow unconsciously furrows when I am thinking just looks angry. I can now see some humor in the fact that my thinking face has been the cause of more than one conflict in my life). Just a minute earlier I had thought about how I enjoyed the smell of burning leaves as the neighbors lit their pile. The wind was gently blowing toward my office. The whole office smelled like a yardwork-Saturday in November. Their smoke increased the number of submicron particles in my office tenfold. Directional airflow matters when it comes to submicron particles and our safety. I haven’t been able to make good sense of the data we have collected. But it doesn’t seem like the typical procedures in my practice using an electric surgical handpiece or even piezo-surgical instruments significantly increases the number of submicron particles more than six inches from the surgical field. My loops keep me at about 20 inches. Hopefully this indicates some level of safety from the threat of SARS CoV-2 which has been reported to hitch a ride on the 0.3-micron particles described as aerosol. It is comforting knowing that there are so many sharp minds working diligently around the world to increase our understanding of this novel virus. As new information is presented, I find myself trying to assimilate it with the practical.
Smoke follows beauty. Protect the beautiful things in your life.
Day 10: Wishes
I often find myself paralyzed if I don’t know the next steps. I had become comfortable thinking that I could usually figure out adequate or even great solutions to most problems with enough information and guidance. We live in an answer driven world. But now more than ever I am finding that the answers aren’t always so clear. I don’t like to take a step unless I am confident in my footing. And rightfully so. My world as a private practice oral surgeon demands a certain level of knowledge, experience and confidence. I am learning more and more to honor tension and give space for it. Tension between risk and benefit. Evidence and opinion. Confidence and humility. Knowledge and teachability.
“None of us is as smart as all of us.” is a common phrase around here. I lean on my team. Together we explore new problems and potential solutions. It has been a challenging and imperfect process. But it is the culture I want. I value my team. They are smart. They care. They see things from a different perspective.
The conversation at last week’s Tuesday morning meeting started with a simple question: “what do you wish for?” I wanted to know what the people on my team are dealing with. What they observe. How they feel. How patients feel. They opened up. It felt good. I want to share some of what I heard from my team.
Everyone agreed that they wish they could see their family. Some have given up more than others. It is hard to choose to distance from an elderly parent fearing what could happen if they unknowingly shared the virus.
“I wish I could go out to eat again.” someone said.
“I just want to want to go out to eat. Right now, I am nervous about it.” another added.
One family had already ventured out to a restaurant, following our local guidelines. She said it felt really good, and the service was amazing. “We were our server’s only table that night.”
“I wish there was no social media.” I listened as they shared their perspective on the positive and negative aspects of social media. My team was frustrated that many people accept opinions as facts on social media. It has become the primary source of information for much of our population. And it is often very manipulative. It does provide a valuable connection with family and friends during this disconnected time. There is a sense of deep connection when someone shares common struggles. They don’t feel as alone. And it raises awareness about some realities missed by typical media outlets.
Our kids are resilient. We all wish the best for them. There is a sense of concern for how this will impact them.
What is hard about the new normal?
“Normal doesn’t seem like the right word.” We discussed what normal means and decided we don’t really want a new normal. We were fond of just normal.
Not sleeping in
Getting back into a routine. But it feels good to be in a routine
PPE
Trying to function without good advice on how to function. It feels like everyone is trying to impose their opinion on you
Counseling patients on things outside of our typical surgical discussion. It takes a lot more time. People open up a lot more when we ask them how they are doing. It used to be a one-word response. Now they actually tell us how they are doing.
Masks are physically tiring. We wear them all day long and then must wear them everywhere else we go.
Patients
Patients are harder than ever to read. We used to be able to tell within 30 seconds how anxious or calm a patient was. Now we can only read their eyes. It makes it much more difficult to meet them where they are at.
They silently observe. It seems like they are watching everything we do. Much of it is the same as it has always been. But now they are watching to see if we use hand sanitizer when we come and go. They notice our safety now more than before.
It isn’t our office or team that they are afraid of. They are afraid of each other.
Some are afraid of everything. They act like you are shooting them when you take their temperature. It is as though the clipboard is made of radioactive material. The chairs are covered with poison. We have had to adapt to new fears. Our conversations have changed. “If that is what makes you comfortable.” seems to go a long way when confronting a patient's fears. We just let them know we will do anything we can to make them feel comfortable. The calm atmosphere is reassuring. Frantic begets frantic. Calm begets calm. It is super important.
Some seem angry. You might as well handcuff them and take away their freedom if you are going to request that they wear a mask during their appointment.
Most don’t seem afraid. They trust that we are doing the best we can. They are gracious and appreciative of the efforts we are taking. They are more patient if we are running behind or can’t get them worked into the schedule as soon.
The questions are different. On the phone they ask about the details. What steps are we taking? How has the facility changed? They are trying to figure out if it is safe. When they get here, they ask about us. They are concerned for us. They want to know how we got through it. They care about how we have been impacted personally. It is a different level of connection.
Team
It feels good knowing that we are all doing our part to keep up to date. We talk with each other about what we are learning. That builds our confidence in the team. We are taking steps to be safe. It is not a guarantee, but we need to do our job.
Thorough screening of the patients and ourselves makes it a lot easier to come to work. It feels safe.
We all want to know that we are doing the best we can. We are cautious and grounded. Not over the top. Intellectual but not hyper focused. We all need to be here. Our patients need us to be here. So, we continue to show up and do our best.

 By:
By: