Implant rehabilitation in the edentulous upper jaw can be achieved with fixed and removable prostheses. Fixed prostheses are totally supported by implants, whereas removable prostheses can be supported by the mucosa with implant retention or totally supported by an implant. In totally edentulous patients, fixed implant rehabilitation shows higher survival rates compared with removable prostheses (1).
The possibility of rehabilitating an arch with a fixed prosthesis with predictable long-term success has been an important goal in dentistry (2). However, the rehabilitation of a completely edentulous maxilla is often associated with anatomical limitations from decreased bone volume, especially in the premolar and molar regions. Bone atrophy progresses rapidly during the first year after tooth loss and continues thereafter. It is affected by long-term use of removable prostheses and relative maxillary sinus pneumatization (3).
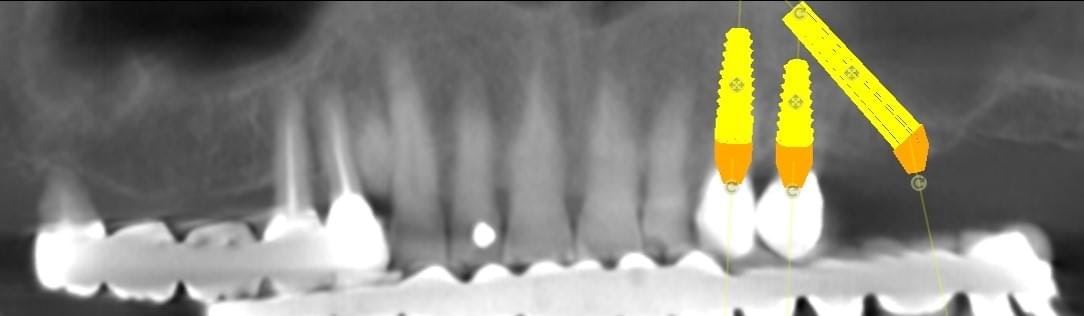
For moderate to severe maxillary atrophy, in the presence of surgically challenging sinus anatomy, the apex of the posterior implants can be angled anteriorly, passing transsinus, to apically fix at the lateral piriform rim into the lateral nasal wall. The most important bone for apical fixation of implants in this setting is the lateral nasal bone mass with the maximum available bone found at the piriform rim above the nasal fossa (4,5). This area, designated the M point, also can engage two implants placed at 30-degree angles (Figs. 1a-b). The transsinus implants are then grafted and possibly placed into immediate function, depending on the level of crestal stability present.
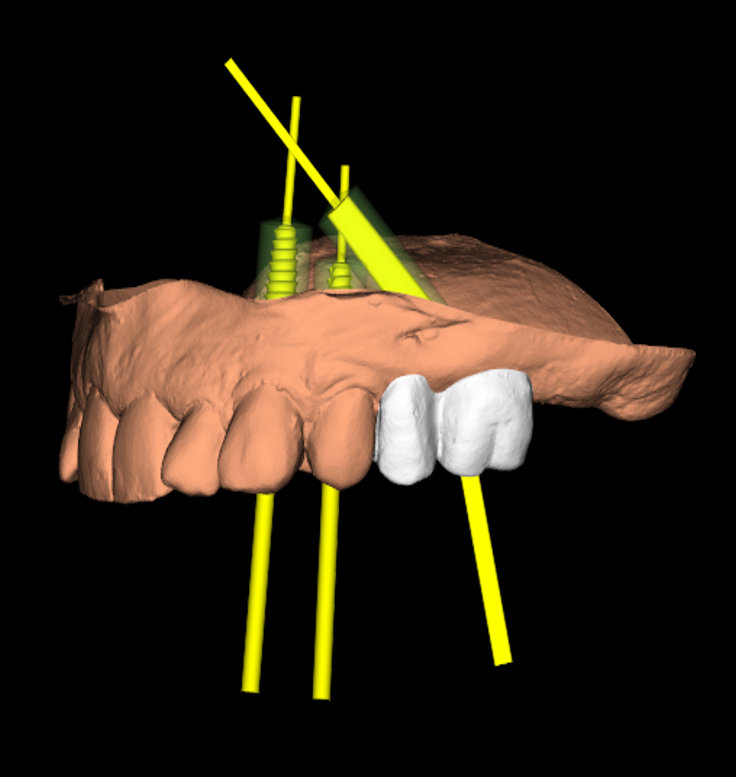
Digital implant project: three different views of the same procedures.
Surgical Procedure
An incision is made along the crest with vertical releasing incisions to obtain access to the lateral and anterior walls of the sinus. The extension of the flap is smaller than a traditional sinus elevation. Once a full-thickness flap is elevated, a small antrostomy is made parallel to the anterior sinus wall starting 3 mm distal to it and then extending anteriorly to reach the anterior sinus wall. The antrostomy is usually 4 to 6 mm mesiodistally and 7 to 8 mm apicocoronally. This simplified antrostomy design is preferred because extension of the antrostomy to the anterior wall renders the membrane elevation procedure simpler and safer by providing direct visual access to the narrow anterior portion of the sinus. This results in a reduced membrane perforation rate (Fig 2a-b).
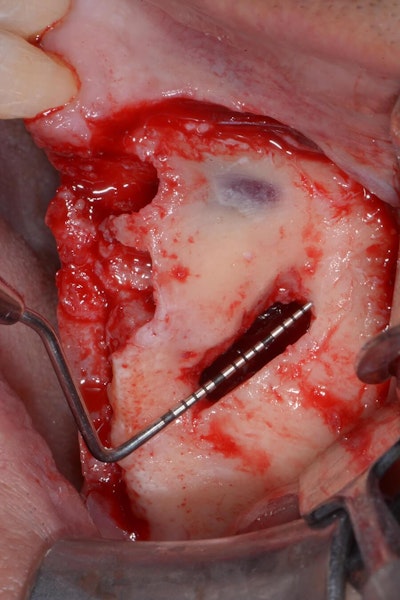
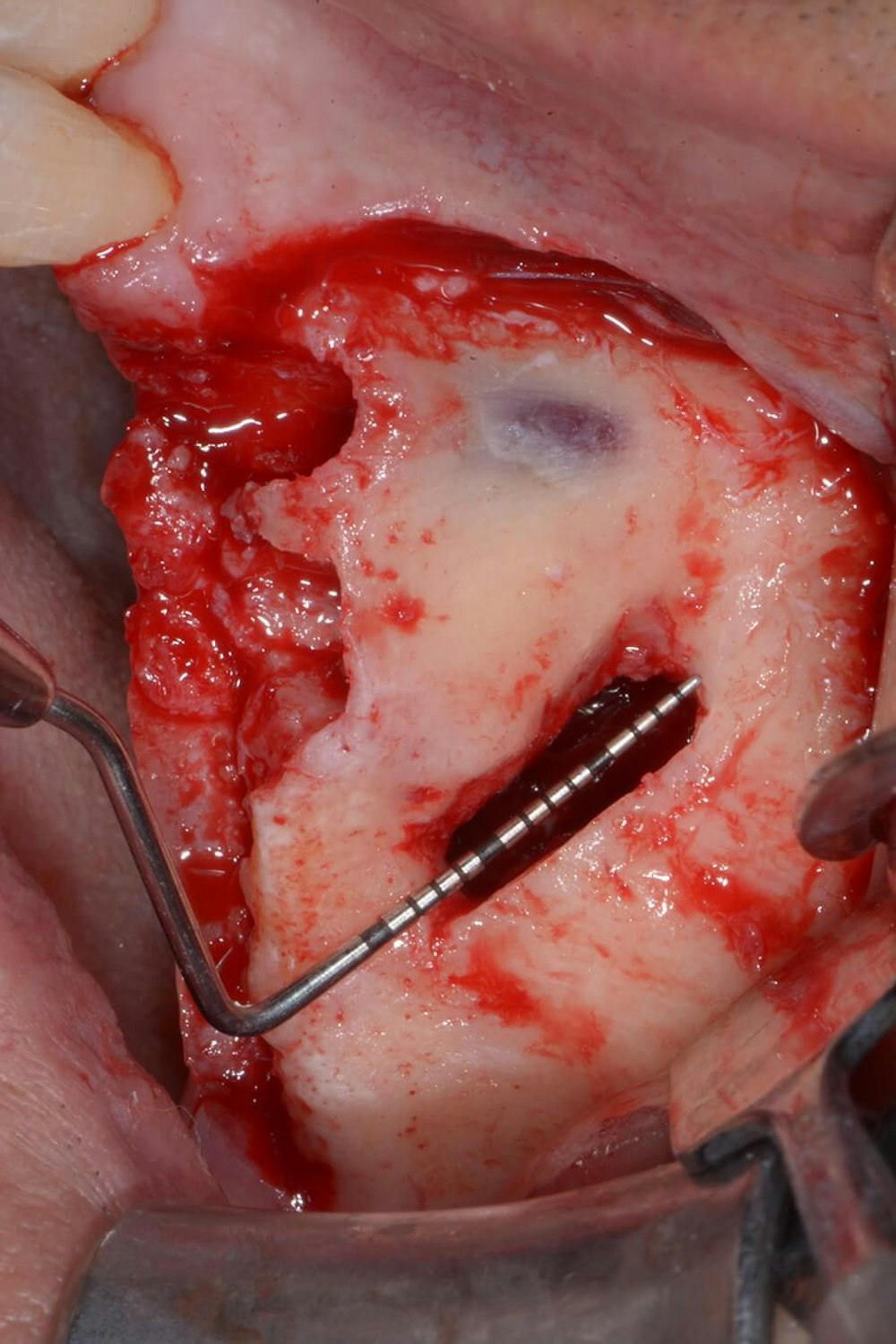
The antrostomy is parallel to the anterior sinus wall. The membrane has been distally displaced and the nasal mucosa is gently elevated to allow implant site preparation.
The approach is accomplished by using a three step procedure:
1. Make a small window 3 mm wide by 6 mm long just distal to the location of the anterior sinus wall correlated with the CBCT scan.
2. Extend the window in the anterior direction to locate the anterior sinus wall.
3. Detach the sinus membrane from the anterior wall, always maintaining instrument contact with the bone, and push the membrane distally.
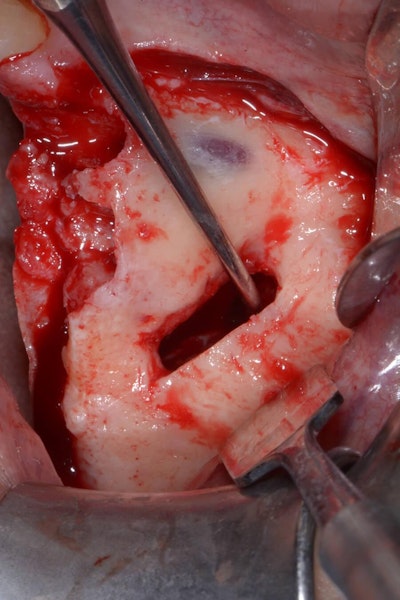
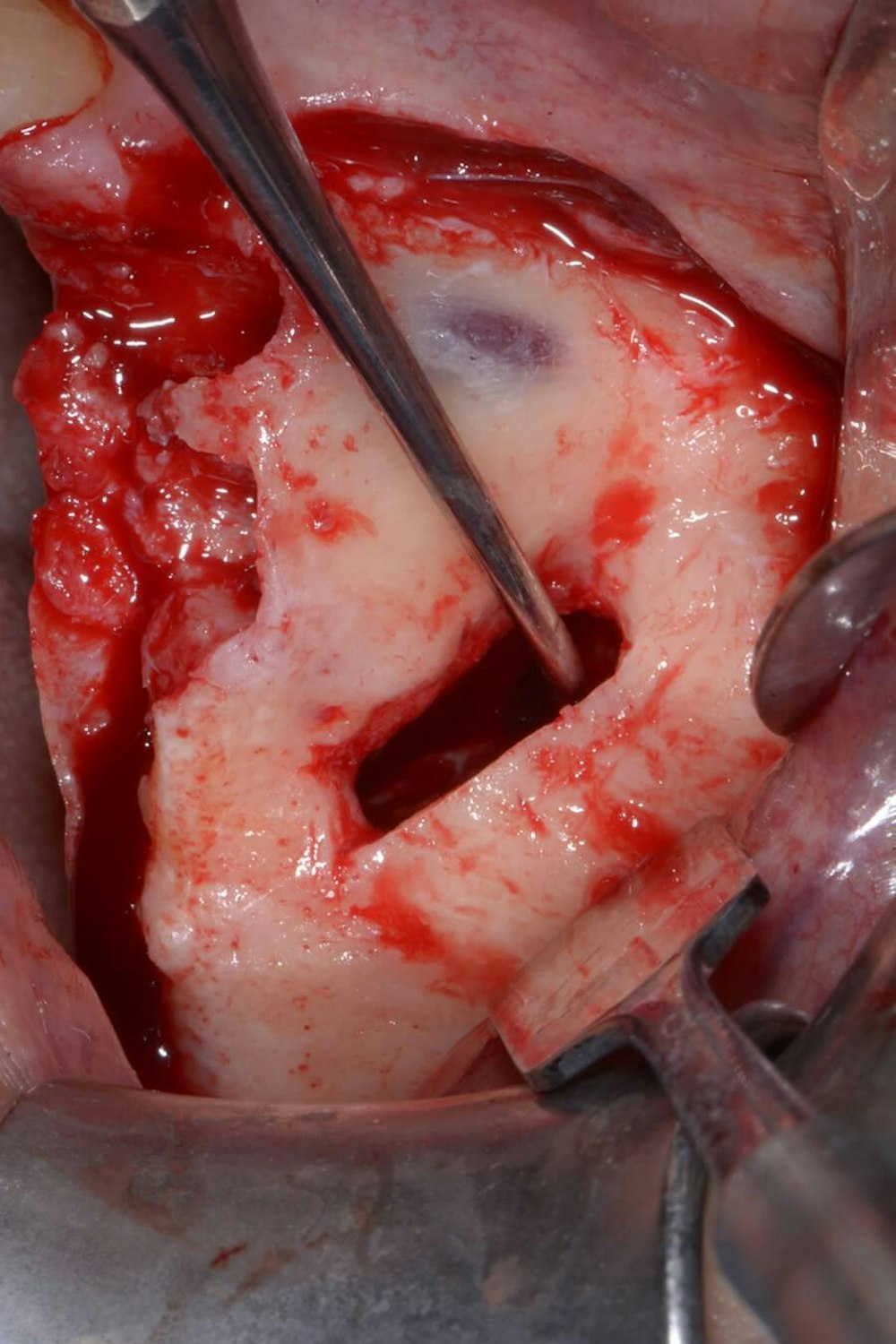
Distal displacement of the sinus membrane allows for the placement of an implant with a distal tilt of 30 degrees (Fig. 3). The direction of the first implant drill can be observed through the antrostomy. The preparation of the implant site extends apically through the anterior sinus wall into the cortical layer of the often adjoining lateral nasal wall. After verification of the implant axis using direction indicators, the drilling sequence is finalized and a bone substitute is inserted (on average, 1 mL of graft material is needed). The implant is then inserted through the residual crestal bone into the grafted sinus where the membrane has been previously displaced distally. It engages apically at the M point, the confluence of three cortical walls. In some cases, it may be possible to obtain satisfactory implant stability without engaging the lateral nasal wall cortex. This approach further simplifies the surgical procedure.

The implant drill is used at a 30 degree angle.
Conclusions
The rationale of this surgical technique is to use the tilted implant approach not only in native bone, but also in conjunction with sinus membrane distal displacement to allow a fixed prosthetic rehabilitation (Figs. 4a-d).



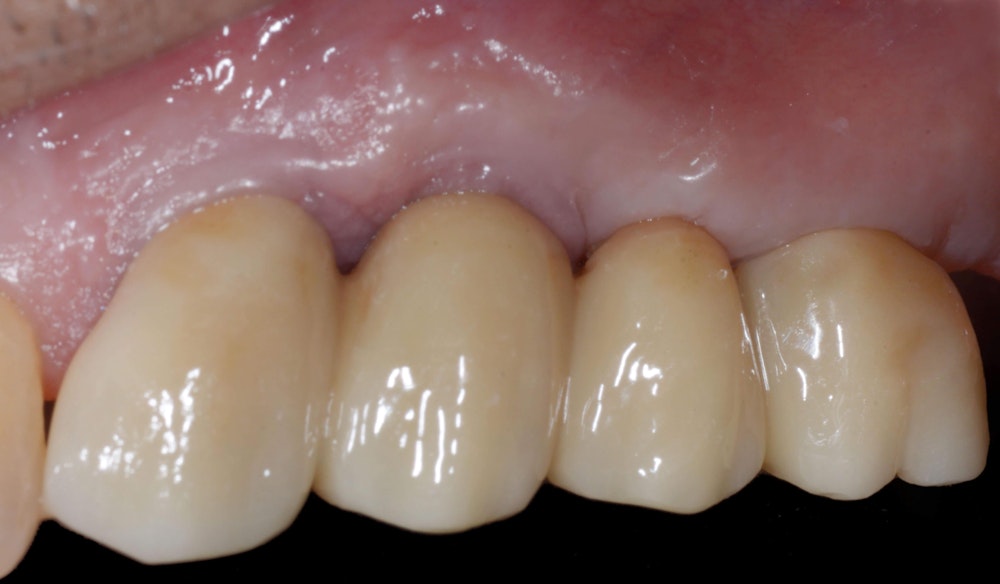
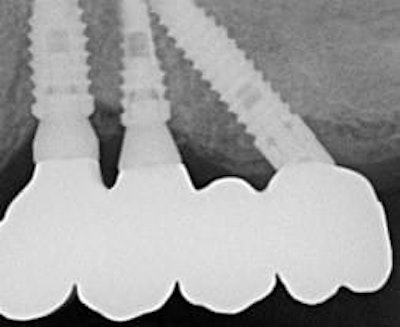
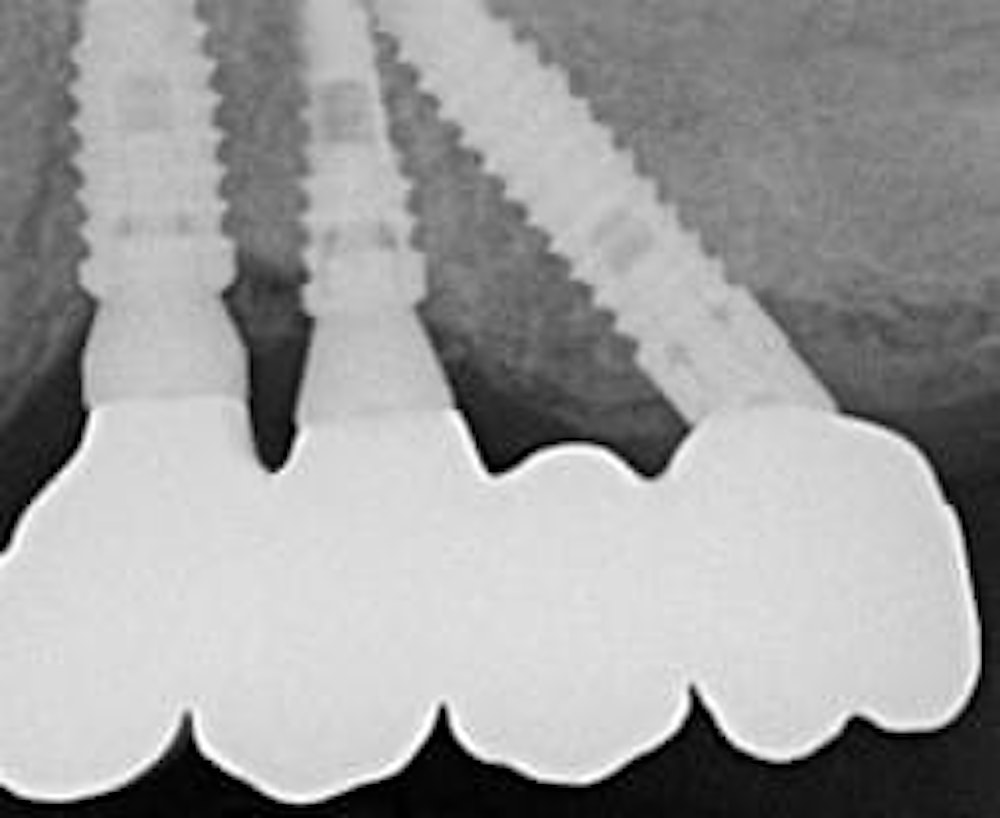
Occlusal and buccal vision of the final prostheses.
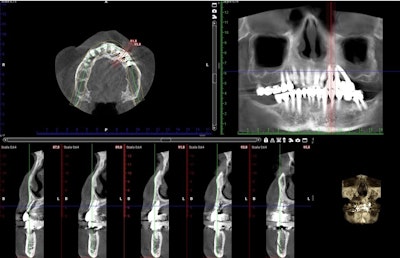
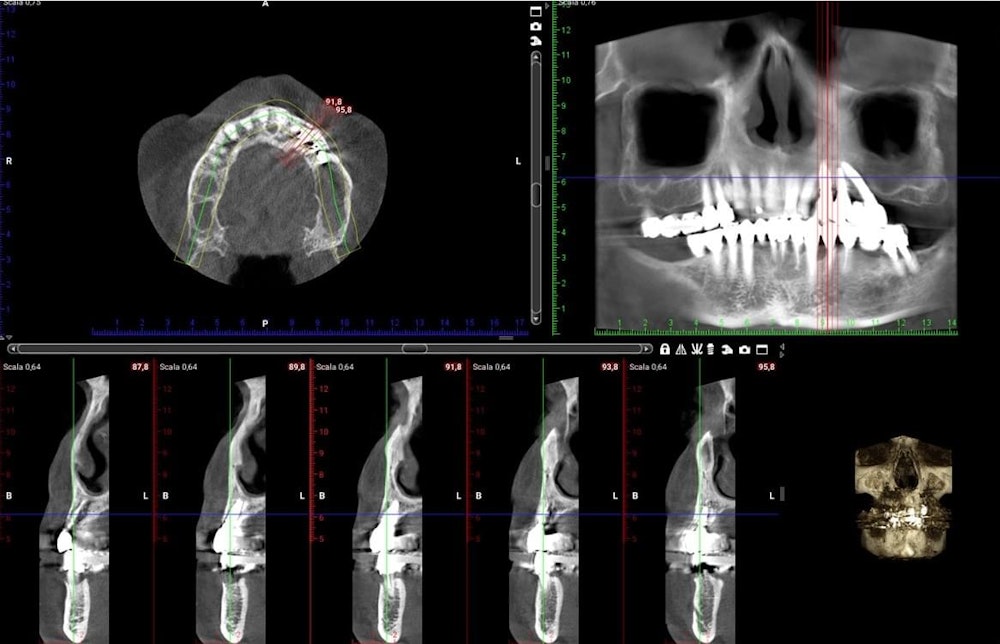
X-ray and CBCT post-op.
Many studies have emphasized that bone density is an important factor for implant success (6,7). The technique proposed in this article targets implant stabilization in three layers of cortical bone: the cortical layer at the osseous crest of the alveolar process, the cortical layer at the floor of the maxillary sinus, and the cortical layer of the anterior sinus wall.
Swelling and bruising seems to be rare in the post-operative period. This finding is likely because of decreased extension of the mucoperiosteal flap elevation when compared with a traditional sinus procedure. The requirement to expose only the anterior wall of the sinus for a small antrostomy and the reduced overall surgical time contribute to reduced morbidity when compared with traditional lateral sinus elevation.
References
1. Jemt T, Book K, Linden B, et al. Failures and complications in 92 consecutively inserted overdentures supported by Branemark implants in severely resorbed edentulous maxillae: A study from prosthetic treatment to first annual check-up. Int J Oral Maxillofac Implants 1992;7:162.
2. Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. IntJ Oral Maxillofac Implants 1990;5:347359.
3. Rossetti PH, Bonachela WC, Rossetti LM. Relevant anatomic and biomechanical studies for implant possibilities on the atrophic maxilla: Critical appraisal and literature review. J Prosthodont 2010;19:449-457.
4. Ma16 P, Nobre Md, Lopes A. Immediate loading of'AII-on-4' maxillary prostheses using traps-sinus tilted implants without sinus bone grafting: A retrospective study reporting the 3-year outcome. Eur J Oral Implantol 2013;6:273-283.
5. Jensen OT, Adams MW The maxillary M-4: A technical and biomechanical note for all-on-4 management of severe maxillary atrophy-Report of 3 cases. J Oral Maxillofac Surg 2009;67:17391744.
6. Ay S, Gursoy UK, Erselcan T, et al: Assessment of mandibular bone mineral density in patient with type 2 diabetes mellitus. Dentomaxillofac Radiol 2005;34:327.
7. Martin W, Lewis E, Nicol A: Local risk factors for implant therapy. Int J Oral Maxillofac Implants 24(suppl) 2009:28.
 By:
By: