We often think of tooth wear as a natural part of aging; teeth flattened by attrition, incisors shortening with age and teeth developing wear facets. Isn’t it just a function of time and circumstance in the mouth?
While some tooth wear is a natural part of aging there is growing evidence of pathological tooth wear in populations, with erosion providing an overlay that accelerates wear, unrelated to a patient's age. Accelerated tooth surface loss has aesthetic, functional and biomechanical implications for patients and if the condition is not recognized and the aetiology addressed, it may continue unabated with negative sequelae. By the time the dentist or patient is aware of the problem, wear can be advanced and solutions complex and costly.
Tooth wear begins as a reduction in the thickness of enamel due to intrinsic and extrinsic biological and chemical factors which do not include caries or trauma. It is also a function of motion and lubrication, accelerated in xerostomia. The term tribology is used in the scientific world to explain the complex mechanisms involved in frictional wear.
When do we need to be concerned about tooth wear in general practice?
Starting with Differentiation.
The first step in adding a tooth wear assessment to your new patient visit is to recognize different patterns of wear.
Tooth wear can be differentiated as:
Attrition
Abrasion
Abfraction
Ablation
Erosion
Each form of tooth wear has a distinct pattern when we observe affected teeth. However, it is common to observe erosion in combination with other forms of wear, confounding the diagnosis. That requires us to become dental detectives, with keen observational skills and an ability to look beyond a standard medical or dental history for clues about aetiology.
For example, becoming familiar with medication that induces xerostomia or bruxism, or understanding silent reflux symptoms can help to clarify factors that may contribute to tooth wear.
Medical and Dental History
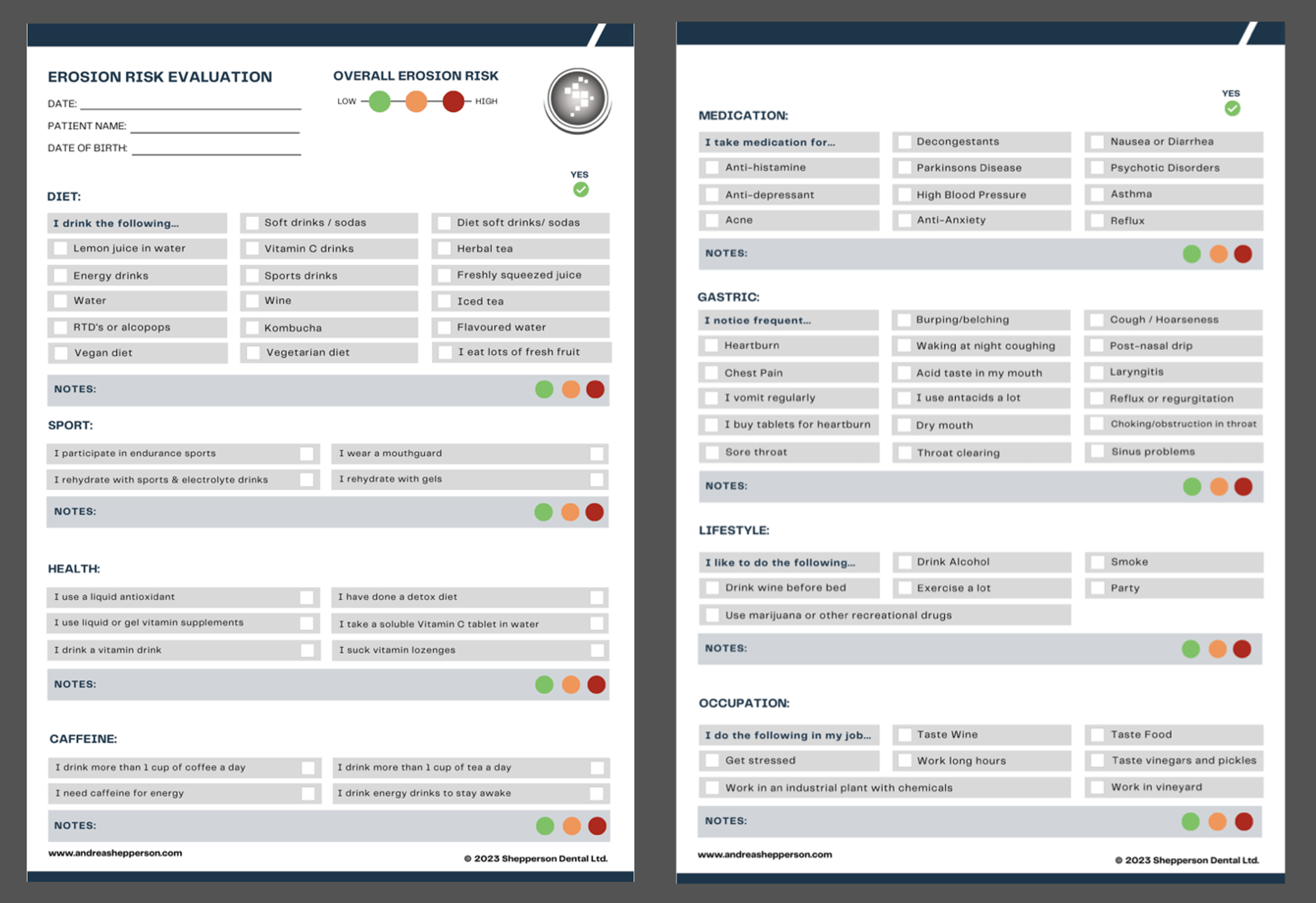
Assessing information provided by the patient often involves further investigation, expanding on patient responses with additional questions as we correlate clinical observations of wear with a patient history. The use of a risk assessment checklist, completed by the patient, can help to direct questions and elucidate a more thorough lifestyle or medical aetiology for tooth wear.
The Aetiology of Tooth Wear
When we understand the mechanisms at play, we can decipher an aetiology. Familiarity with both intrinsic and extrinsic forms of erosion, new classifications for sleep and awake bruxism, recognizing GERD as a spectrum of disorders, the link between GERD and OSA and the wide array of dietary and lifestyle factors will aid in distinguishing a pattern of wear. Sometimes the aetiology is not always obvious or may mimic other patterns of wear.
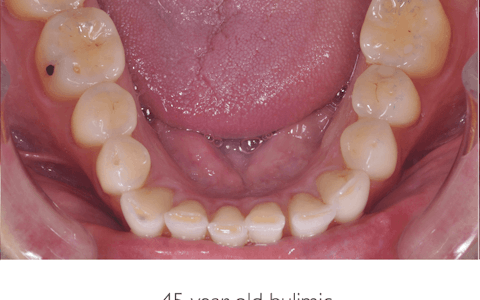
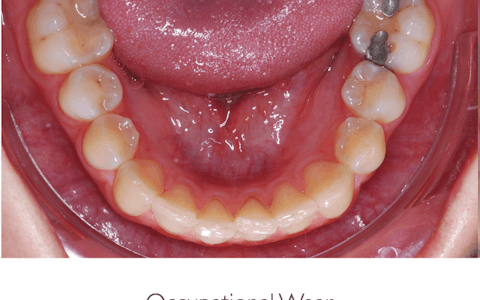
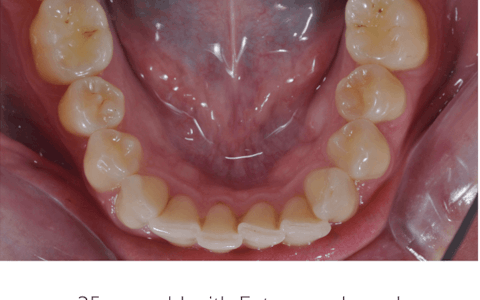
The images below show 3 similar patterns of erosive wear, with very different aetiologies. Taking the time to explore the patient’s history and habits will help to pinpoint the origin of wear.
What Is a Normal Rate of Wear?
How do we determine pathological from physiological wear? In evaluating the mechanisms of wear, attrition and abrasion are physiological. Tooth wear and the attrition patterns are also used for estimates of age in anthropological studies and in forensic dentistry.
Attrition and abrasion become pathologic when the rate and nature of wear increases the risk of associated pathology. Erosion is generally considered as pathologic and was rarely seen in hunter-gatherer skulls.
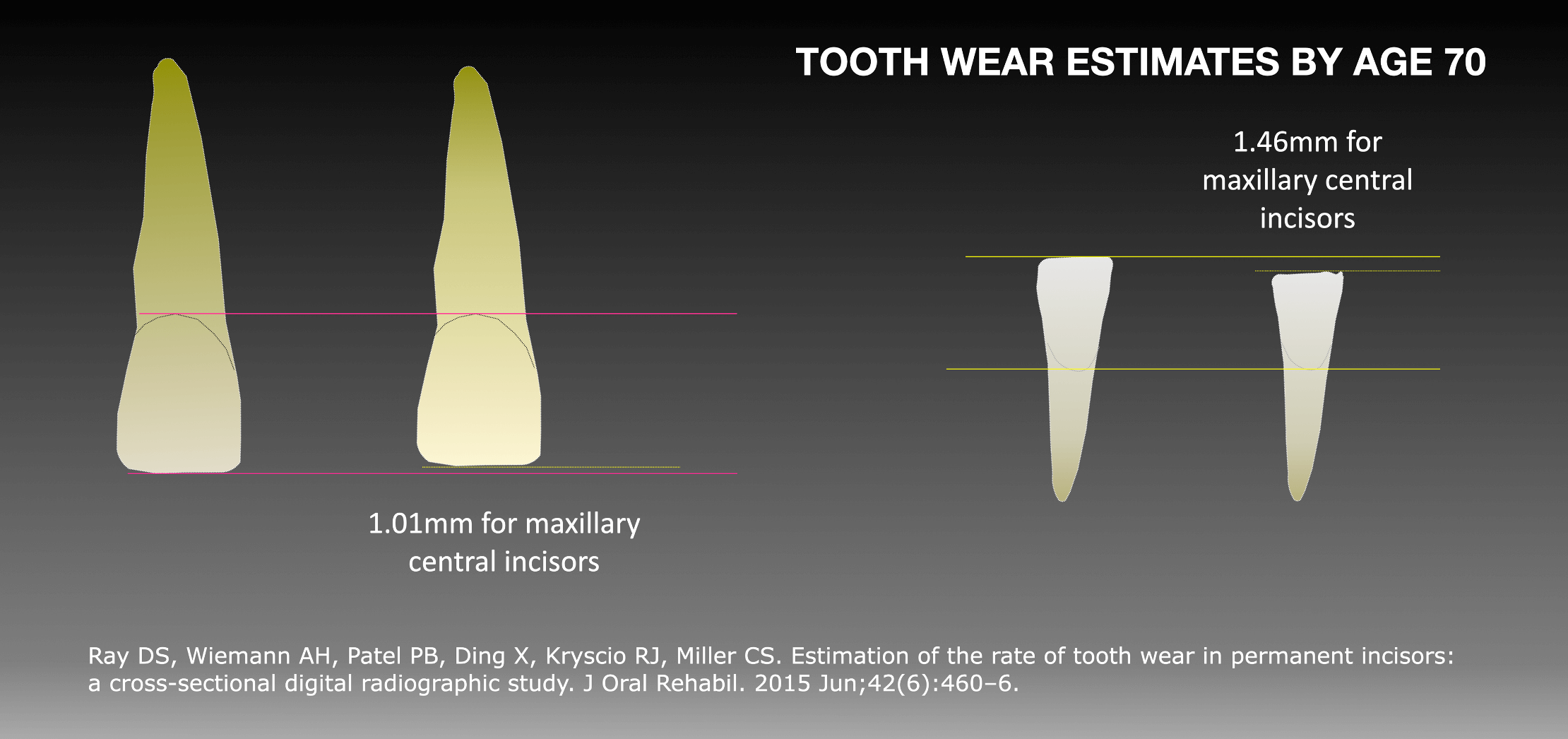
Many studies have been done to assess the rate of tooth wear in populations and the relationship of tooth wear to age. Several qualitative methods and indices have been proposed to measure tooth wear. While there is no global consensus, some studies have been cited as a benchmark in determining and classifying pathological wear. Ray et al. quantified tooth wear and used conventional digital radiography to estimate the rate of tooth wear of maxillary and mandibular central incisors. Tooth wear was estimated to average 1.01 mm for maxillary central incisors and 1.46 mm for mandibular central incisors by 70 years of age.
In 2016, leaders in the field of tooth wear research met to develop the European Consensus Statement on the management of severe tooth wear, including a flow chart and decision tree to help dentists determine when to monitor and when to intervene.
The Consensus Statement defined severe wear versus pathological wear:
1. Severe Tooth Wear
Tooth wear with substantial loss of tooth structure, with dentin exposure and significant loss
(≥1/3) of the clinical crown. It is unlikely to be active wear. For example, an older patient may present with severe tooth wear that poses no concern to the patient
2. Pathological Tooth Wear
Tooth wear that is active wear and atypical for the age of the patient, causing pain or discomfort, functional problems, or deterioration of aesthetic appearance, which, if it progresses, may give rise to undesirable complications of increasing complexity., providing dentists with a flowchart that helps in providing advice to patients and guiding the need for treatment.
The risk of ignoring tooth wear and carrying out extensive restorative treatment in a worn dentition without exploring the cause, rate of wear, or raising the consequences with the patient creates the potential for:
Ongoing tooth wear and structural fatigue in the presence of chemical or biomechanical forces.
Failure of newly placed restorations.
The risk of sensitivity, pulpal involvement, or tooth loss.
Aesthetic compromise.
Anterior teeth are under increasing load and risk of failure, where posterior wear is active.
Costly re-treatment for the patient.
___________________________________________________________
To learn more about Tooth Wear, check out Dr. Shepperson's book "Managing Tooth Wear: A Comprehensive Guide For General Practice"
This comprehensive guide is designed to empower dental professionals by offering invaluable insights into the intricate world of tooth wear. It delves deep into the intricacies of recognizing and addressing this common issue, providing you with the expertise to make informed clinical decisions.
Master the art of differentiation between essential and non-essential treatments. Gain a profound understanding of the fine line between physiologic and pathologic wear, equipping you with the skills to guide your patients towards optimal oral health without resorting to unnecessary interventions. Discover the potency of interdisciplinary dentistry, incorporating orthodontics and other conservative alternatives to provide less invasive solutions.
"Managing Tooth Wear" leaves no stone unturned when it comes to tooth wear management. It offers a holistic view of treatment options, equipping you with the insight to motivate and guide your patients effectively. Prioritizing biological, functional, and ethical rationales, this book ensures that enamel conservation and protection remain at the forefront of your practice.
 By: Dr. Andrea Shepperson
By: Dr. Andrea Shepperson