When new drugs that are likely to gain significant popularity appear on the market, particularly those associated with bleeding diathesis, it is important for dentists to become familiar with these drugs and to understand the best way to manage patients using them when they need dental interventions.
While most dentists are comfortable managing patients on Coumadin, they are probably just beginning to see patients who are taking the four newer oral anticoagulants (NOACs): Pradaxa (dabigatran), Xarelto (rivaroxaban), Eliquis (apixan) and Savaysa (edoxaban). These agents have been approved for use in anticoagulating patients with non-valvular atrial fibrillation (AF), Deep vein thrombosis (DVT), pulmonary embolism (PE) and for post-operative prevention of DVT after hip and knee surgery.
Much like for patients taking Coumadin (Warfarin), these drugs can be continued for simple dental procedures. In instances where complicated dental procedures are planned, it’s critical to consult with the patient’s physician to discuss the feasibility of temporarily withholding these drugs to avoid excessive bleeding.
To intelligently manage these patients in the dental setting, it’s important to understand the indications for NOACs, their mechanisms of action, their advantages and their disadvantages.
INDICATIONS FOR NEW ORAL ANTICOAGULANTS
Many patients are on the oral anticoagulant Coumadin (Warfarin) for non-valvular AF, DVT, PE and to prevent DVT after hip and knee surgery.
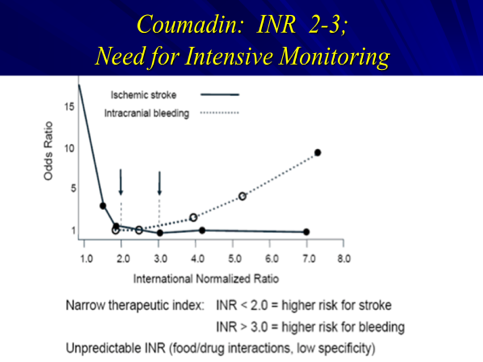
AF puts patients at 17 times the risk for stroke; Coumadin significantly decreases that risk (Figure 1). However, over-anticoagulation can result in bleeding complications, including hemorrhagic stroke. Patients on Coumadin are carefully monitored by prothrombin time/international normalized ratio (PT/INR). Their dose continuously changes according to the INR value. Patients and physicians have found this process tedious and inconvenient, so there has been a continuous search for agents that can more precisely titrate the degree of anticoagulation. This has resulted in the development of drugs that can be given in a fixed dose without continuous monitoring.
Figure 1: Coumadin and Stroke
The four NOACs have been approved for use in patients with non-valvular AF, DVT, PE and for preventing DVT following hip and knee surgery. In essence, with the exception of anticoagulation for mechanical valves, NOACs now cover every indication for which Coumadin is traditionally prescribed.
MECHANISM OF ACTION OF TRADITIONAL AND THE NEWER ORAL ANTICOAGULANTS
The new oral anticoagulants work at sites different from Coumadin and are gaining acceptance because of their ease of use.
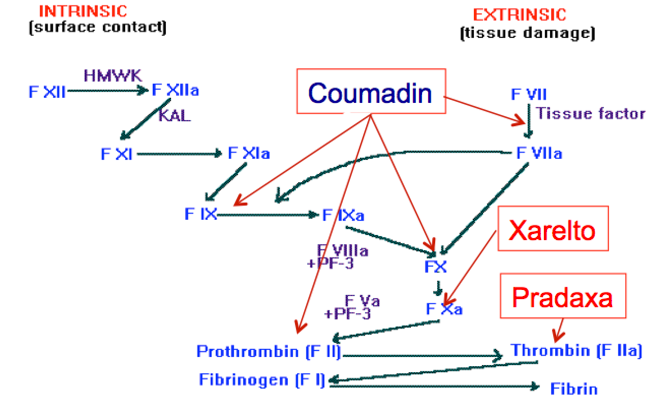
Coumadin interferes with coagulation by acting on four vitamin-K dependent coagulation factors (Figure 2). These factors are quite sensitive to changes in vitamin K availability. Minor changes in diet or the use of antibiotics can affect these factors. It is therefore important to meticulously manage the level of anticoagulation (measured by PT/INR) in patients on Coumadin. Doses have to be carefully adjusted.
Unlike Coumadin, NOACs act at sites quite close to the formation of the fibrin clot (Figure 2). The level of anticoagulation is therefore more predictable and the drugs can be given at a fixed dose without monitoring blood tests. There are also no dietary restrictions with these agents (Table 1). Patients and physicians find these features attractive and an increasing number of patients are now on Pradaxa and Xarelto.
Figure 2. Sites of Action of Coumadin, Xarelto, Eliquis, Savaysa (Factor Xa) and Pradaxa (Factor II)
In clinical trials, all NOAC agents have been as or more efficacious than Coumadin in preventing stroke in patients with non-valvular AF, in managing DVT or PE and in preventing DVT after hip and knee surgeries. In these trials, patients had fewer bleeding complications with the NOAC agents than with Coumadin.
Table 1. Comparison of Coumadin and NOACs
Coumadin (Warfarin)
|
Pradaxa (Dabigatran) |
Xarelto (rivaroxaban)
|
Eliquis (apixan) |
Savaysa (edoxaban) |
Requires regular blood tests | No need for regular blood monitoring | No need for regular blood monitoring | No need for regular blood monitoring | No need for regular blood monitoring |
Some dietary restrictions | No restrictions | No restrictions |
No restriction |
No restriction |
Dose available | 75 mg or 150 mg |
10 mg or 15 mg
|
2.5 mg or 5 mg |
60 mg |
Taken once a day | Twice a day |
Once a day (evening)
|
Twice a day |
Once a day |
Variable dose according to PT/INR | Fixed dose | Fixed dose |
Fixed dose |
Fixed dose |
REVERSAL AGENTS
Significant clinical bleeding in patients using Coumadin can be reversed with vitamin K or fresh frozen plasma. We now have reversal agents for all NOACs. Praxbind (idarucizumab), a monoclonal antibody, binds and negates the effect of Pradaxa. Andexanet alpha, a decoy Factor Xa, can reverse the effects of Xarelto, Eliquis and Savaysa.
Equally importantly, NOACs have relatively short half-lives. In general, NOACs are held when there is clinically significant bleeding. Patients rarely need reversal and even more rarely need blood transfusion.
BLEEDING COMPLICATIONS OF THE NEW ORAL ANTICOAGULANTS
Like Coumadin, all NOACs can be associated with bleeding complications.
Pradaxa, Xarelto and Eliquis are cleared by the kidneys. The risk of bleeding is higher in patients:
75 years old or older
with renal dysfunction
with a history of gastrointestinal bleeding
on anti-inflammatory drugs
on aspirin products
on certain drugs
Eliquis has the advantage of not being renally cleared. The risk of bleeding is higher in patients:
with liver dysfunction
on anti-inflammatory drugs
on aspirin products
on certain drugs
None of the NOACs are approved for use in pregnant females or nursing mothers.
DENTAL MANAGEMENT OF PATIENTS ON NOACs
I have reprinted a page from the Ultimate Cheat Sheets: A Practical Guide for Dentists that covers managing patients on Pradaxa as a quick reference for dental management (Figure 3).
Figure 3. Dental Management of Patients on Dabigatran (Pradaxa)
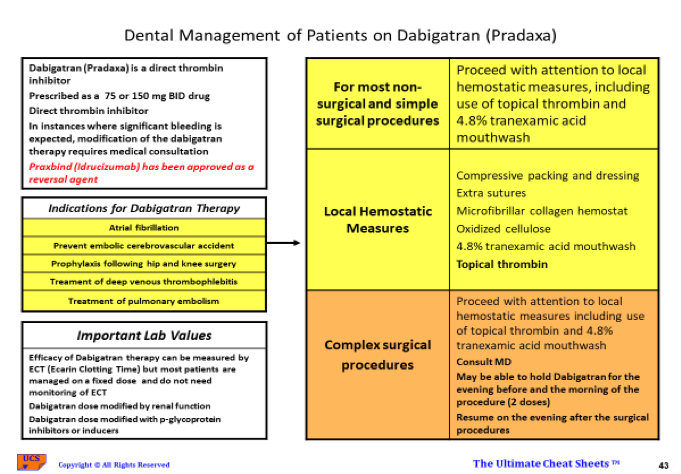
Although the degree of anticoagulation by NOACs can be measured by Ecarin Clotting Time (ECT), this test is rarely necessary because all the drugs give relatively predictable levels of anticoagulation. Dentists must decide whether it’s necessary to interrupt anticoagulation therapy. This depends on the procedure planned, the clinical scenario and the likelihood of bleeding complications.
For most non-surgical and simple surgical procedures, it’s reasonable to proceed with attention to local hemostatic measures without interrupting therapy. This is based on an analogy drawn from managing patients on Coumadin, where interrupting Coumadin was found to have more risk than benefit. However, keep in mind NOACs have much faster onset and washout than Coumadin and relatively short half-life.
A patient who is taken off either agent for 24 hours has a very short period with lessened anticoagulation. The risk of thrombus formation in patients during this short window is low. It is therefore theoretically safer to interrupt NOAC therapy than Coumadin therapy. However, the risk benefit ratio of transient interruption of therapy has not been clearly defined. It is important to include the patient’s physician in any decision that involves interrupting anticoagulation. Patients with significant risk of thrombosis have to be managed without interruption of therapy by careful use of local hemostatic measures.
Local hemostatic measures should include:
Extra sutures
Compressive packing and dressing
Microfibrillar collagen hemostat
Oxidized cellulose
4.8% tranexaminic acid mouthwash
Tropical thrombin
For complex surgical procedures, it’s reasonable to consult with the patient’s physician to see if it is safe to interrupt NOAC therapy.
For Pradaxa and Eliquis (BID drugs), the oral anticoagulant should be held the evening before the procedure and the morning of the procedure. Pradaxa and Eliquis should be resumed the evening after the procedure.
For Xarelto and Savaysa (QD drugs usually given in the evening), the medication should be held the evening before the procedure and resumed on the evening after the procedure.
In all instances, there is still residual anticoagulation and the patients should be warned about issues with hemostasis, but the short period of interruption should decrease the bleeding tendency.
ONE SHOULD NOT STOP ORAL ANTICOAGULANTS WITHOUT DOCUMENTATION OF THE OPINION OF THE MEDICAL CONSULTANTS
If the consulting physician deems the risk of interrupting the oral anticoagulants outweighs the benefit, it is then up to the dental professional to decide if the intended procedures can be done safely in the presence of full anticoagulation.
USE OF COMMONLY PRESCRIBED DRUGS IN DENTISTRY FOR PATIENTS ON NOACs
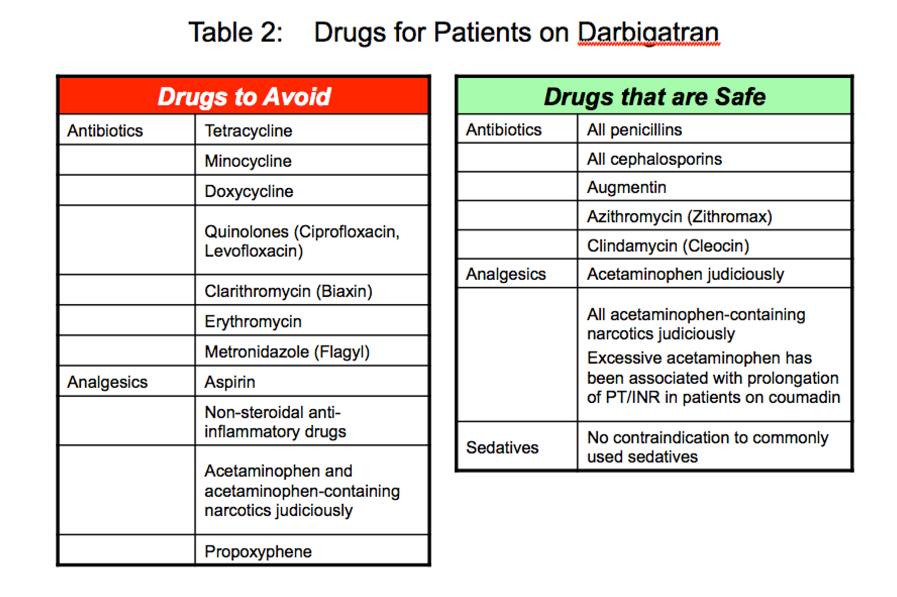
As is often the case, dental professionals should be aware of potential drug-drug interactions with these new oral anticoagulants. Drugs that interfere with the metabolism of these drugs should be avoided. Similarly, drugs that can increase bleeding complications also should be avoided.
I have included a page from the Ultimate Cheat Sheets for drugs that are safe to use and drugs that should be avoided in patients on Pradaxa (Table 2). Only drugs commonly prescribed by dentists are included. In instances where a drug prescribed is not on the list, it’s important to consult a source such as Lexicomp to be sure there is no drug-drug interactions with Pradaxa and Xarelto.
ACCEPTANCE OF THE NEWER ORAL ANTICOAGULANTS (NOACs)
It is clear the fixed dosage of NOACs, the elimination of PT/INR monitoring and the fact there are no dietary restrictions are attractive for patients and physicians alike. It is generally found in clinical trials that NOACs have similar efficacy and are safer than Coumadin. There is therefore increasing use of NOACs clinically.
The previous concerns that these drugs do not have reversal agents are now addressed with the availability of Praxbind and Decoy Factor Xa.
These drugs are now standard first line therapy for managing patients in AF, with DVT or PE and in the prevention of DVT after hip and knee surgeries.
References
1. Ezekowitz MD, Reilly PA, Nehmiz G, Simmers TA, Nagarakanti R, Parcham-Azad K, Pedersen KE, Lionetti DA, Stangier J, Wallentin L Dabigatran with or without concomitant aspirin compared with warfarin alone in patients with nonvalvular atrial fibrillation (PETRO study). Am J Cardiol 100 , 1419-1426 (2007)
2. Soheir S. Adam, MD; Jennifer R. McDuffie, PhD; Thomas L. Ortel, MD, PhD; and John W. Williams Jr., MD Comparative Effectiveness of Warfarin and New Oral Anticoagulants for the Management of Atrial Fibrillation and Venous Thromboembolism: A Systematic Review. Ann Intern Med. 28 (2012)
 By: Dr. Leslie S.T. Fang, MD PhD
By: Dr. Leslie S.T. Fang, MD PhD




