An estimate is nothing more than a prediction. It is an approximation or projection of something based on experience and/or available information, with the understanding that all the facts remain uncertain. Depending on the content, an estimate can be leveraged to address multiple goals. In the context of endodontics, that leverage comes in the form of digital radiography.
Two-dimensional radiography represents the current standard of care with respect to pre-operative imaging for endodontic purposes. Although cone beam computerized tomography (CBCT) is making its way into the pre-operative endodontic arena, this article focuses on two-dimensional digital radiography as the primary tool for making measurement estimates.
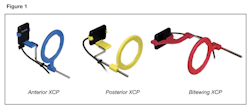
Clinicians should take three pre-operative radiographs for endodontic cases: a straight periapical radiograph, a “cone shifted” periapical radiograph (a radiograph angled 10 to 30 degrees to the mesial or distal) and a bitewing radiograph. Proper image capturing techniques are required to minimize the additional distortion effects of foreshortening and/or elongation. I suggest using an extension cone paralleling device (XCP) (Fig. 1). The images can be used in conjunction with the calibrated digital ruler interface found in most digital radiography software programs.
The Predictive Value of Root Length Estimates
Extensive study of root anatomy and morphology over the decades has provided calculated weighted averages with respect to root length for each tooth in the human dentition as well as each root per tooth. These statistics can be found in most endodontic texts. Averages have value in regards to the anatomical characteristics of a general population, but hold little value for individual patients who require endodontic treatment. Pre-operative root length estimates can be a useful tool when evaluating case difficulty and case selection.
Pre-operative root length is estimated by measuring the distance from the highest point of the occlusal table to the apex of the root being measured. These measurements should be made from the straight periapical radiograph. In multi-rooted teeth, the occlusal table reference point may be different, depending on the location of the root being measured. Often, roots exhibit a degree of curvature, making it difficult to obtain an accurate estimate with a straight measuring tool. If available, I suggest using a multi-angle or polyline ruler function.
It is every clinician’s responsibility to understand individual limitations with respect to case selection. In my experience, the most manageable cases fall within an estimated length range of 17 mm to 21 mm. This length range encompasses the majority of teeth that require treatment. Estimated root lengths within this range allow for convenient use of the electronic apex locator (EAL), the consistent establishment of reproducible reference points, and proper management of length control during instrumentation. Additional factors that may influence case selection should be considered with estimated root lengths of less than 16 mm and/or greater than 21 mm.
Estimated Root Lengths of 16 mm or Less
The greatest challenge with root lengths of 16 mm or less lies with establishing and maintaining accurate working lengths. Many commonly used endodontic files are manufactured with 16 mm of working flutes, generally referred to as the “working portion” of the file (Fig. 2). All working portions are manufactured with a rate of taper, which is the change in file diameter over its length. Silicone file stoppers, used to establish and maintain working length, are manufactured to fit snuggly on the non-working portion of the file, corresponding to its largest diameter. When the stopper is positioned on an area of decreased file diameter, the result is a loose fitting file stopper (Fig. 3).
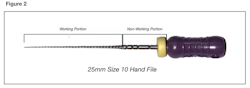
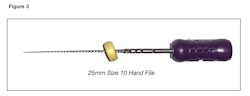
Excessive stopper movement can create inaccuracies when attempting to establish reproducible reference points as well as when measuring the file against an endodontic ruler. Additionally, a loose fitting stopper on an engine driven instrument can give the illusion of proper length control while the file continues advancing apically, leading to over-instrumentation. The shorter the estimated working length, the more dramatic this effect becomes. While this observation may not hold true for every manufactured file, it must be taken into consideration. Recognizing this relationship can improve the odds of proper canal management, but may impact the degree of case difficulty.
Estimated Root Lengths Greater Than 21 mm
Root lengths estimated to exceed 21 mm can impact case difficulty by limiting the clinician to 25 mm files. This may not pose a problem when treating teeth positioned more anterior and/or teeth on patients with an adequate range of joint motion, but when access to a tooth is limited, restrictions on file length options must be taken into consideration when evaluating overall case difficulty.
Estimated Root Lengths Greater Than 23 mm
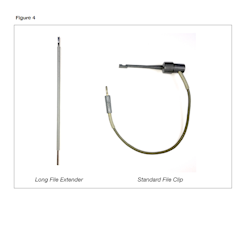
In addition to the limitations mentioned above, estimated root lengths exceeding 23 mm can pose a challenge to using EALs. EALs require available file space above the silicone stopper and below the handle to securely attach the file clip. The available file space required for most EAL file clips is approximately 1.5 mm. When using 25 mm files, the silicone stopper’s position can encroach upon this required file space, impacting the clinician’s ability to predictably secure the file clip and establish an accurate working length.
In this situation, the clinician can choose to use a “long file extender” (Fig. 4), which requires less available file space and/or use 31 mm files. If the latter is chosen, using longer files may not pose an issue unless other limitations are also present, such as limited patient opening and/or the position of the tooth within the arch.
Conclusion
As clinicians, we have the autonomy to perform any treatment that is deemed to fall within our scope of practice. We also are encouraged to push those boundaries with the intent of expanding that scope. Pre-operative root length estimates represent a predictable method for identifying unrecognized challenges that may affect case selection.
 By: Dr. William J. Nudera DDS, MS
By: Dr. William J. Nudera DDS, MS




